ESCRS Breaking News Briefs
Insights & updates from the ESCRS Winter Meeting 2023
A novel high-resolution device capable of performing reliable, precise measurements of ocular aberrations could potentially lead to new screening or follow-up methods for patients with keratoconus or other corneal diseases, according to Gonzalo Velarde-Rodriguez MD.
“The ocular aberrations measured by this device are reliable, precise, and well correlated with the corneal aberrations. Furthermore, the extraordinary high-resolution measurements revealed micro alterations in the wavefront phase of keratoconus patients that varied with the disease stage,” he said.
Dr Velarde-Rodriguez explained the new aberrometer prototype (t-eyede, Wooptix) was developed originally for the astrophysics field with sensors capable of detecting propagating light waves. These sensors allow the user to acquire millions of data points within the pupil of the human eye with a resolution several orders of magnitude higher than current industry standard ophthalmic devices.
Dr Velarde-Rodriguez’s cross-sectional study included 43 eyes from 25 healthy patients and 43 eyes from 27 keratoconus patients analysed by a corneal tomography system and the aberrometer prototype. Corneal aberration values were provided by the tomography device and compared with ocular aberration scores obtained from intensity images captured by the t-eyede device.
Results showed all ocular and corneal optical aberrations were statistically significantly higher in the keratoconus group than the control group. Ocular aberrations were lower than corneal aberrations in both groups, showing a particularly marked difference for astigmatism and coma aberrations—with a reduction of 57% and 51%, respectively.
Visual field progression in open-angle glaucoma (OAG) can be predicted with relatively high accuracy using an artificial intelligence (AI) prediction model applied to measurements obtained using an ultra-high-speed tonometry device (Corvis ST, Oculus), according to a study presented here.
“Visual field progression can be predicted with relatively high accuracy using Corvis ST measurements registered one month after prostaglandin analogues treatment,” said Marta I Martínez-Sánchez MD. “The moment of maximum concavity of the cornea seems crucial for estimating the risk of progression. The early identification of potential fast progressors could have an evident clinical benefit.”
Dr Martínez-Sánchez and co-workers set out to create an AI algorithm to predict the risk of visual field progression in OAG patients using Dynamic Corneal Response (DCR) parameters registered on the Corvis ST before and one, three, or six months after initiating therapy with prostaglandin analogues. The team tested different AI models with a data set of 65 eyes to achieve optimal predictions as measured by their accuracy and area under the curve (AUC). The predictive variables were then analysed to assess which were relevant for final prediction of visual field progression.
The most accurate data predictors were those registered at one-month follow-up, predicting glaucomatous progression with an accuracy of 86.2%. The main variables involved in the prediction were the arc length at the moment of maximum concavity, the time from the deformation onset to the maximum concavity, and the corneal deflection length at the time of maximum concavity. This was consistent across different algorithms, and results did not improve by using additional variables such as corneal hysteresis or IOP values, she said.
Machine learning shows high potential in automatically detecting and classifying dry eye disease (DED), according to Karl Stonecipher MD.
“The models proposed in our study accurately predicted dry eye severity and type,” he said. “Such models may improve health outcomes and provide early alerting to potentially prevent the progression of DED. We are looking at predicted diagnosis and treatment directed towards the diagnosis to improve non-surgical and surgical outcomes.”
Dr Stonecipher explained real-world clinical data captured over 18 months helped to develop two machine-learning diagnostic models for DED severity and type. The data was drawn from more than 25,000 assessments performed in more than 253 clinics currently using the CSI-Dry Eye software—which incorporates the machine learning algorithm. Correlation feature selection (CFS) eliminated redundant and irrelevant features, and Support Vector Machines (SVM) was found to be the best technique to fit the data.
“We developed two SVM models, namely SM (dry eye severity model) and TM (dry eye type model). Both models were successful in predicting different dry eye severity and type cases,” he said.
Dr Stonecipher said incorporating more data will further enhance the performance of the prediction models in the future.
“The more data we put into that machine learning, the better the outcomes,” he concluded.
Cost to the patient, concerns over contrast visual acuity, and night-time quality of vision are the main reasons ophthalmologists cited for not performing more presbyopia IOL procedures, suggests the latest ESCRS Clinical Trends Survey.
Rudy MMA Nuijts MD, PhD, University Eye Clinic Maastricht, Netherlands, presented the latest survey results on the opening day of the ESCRS Winter Meeting.
More than 1,700 delegates responded to 146 survey questions during the 40th ESCRS Annual Congress Milan, the eighth year this survey was conducted.
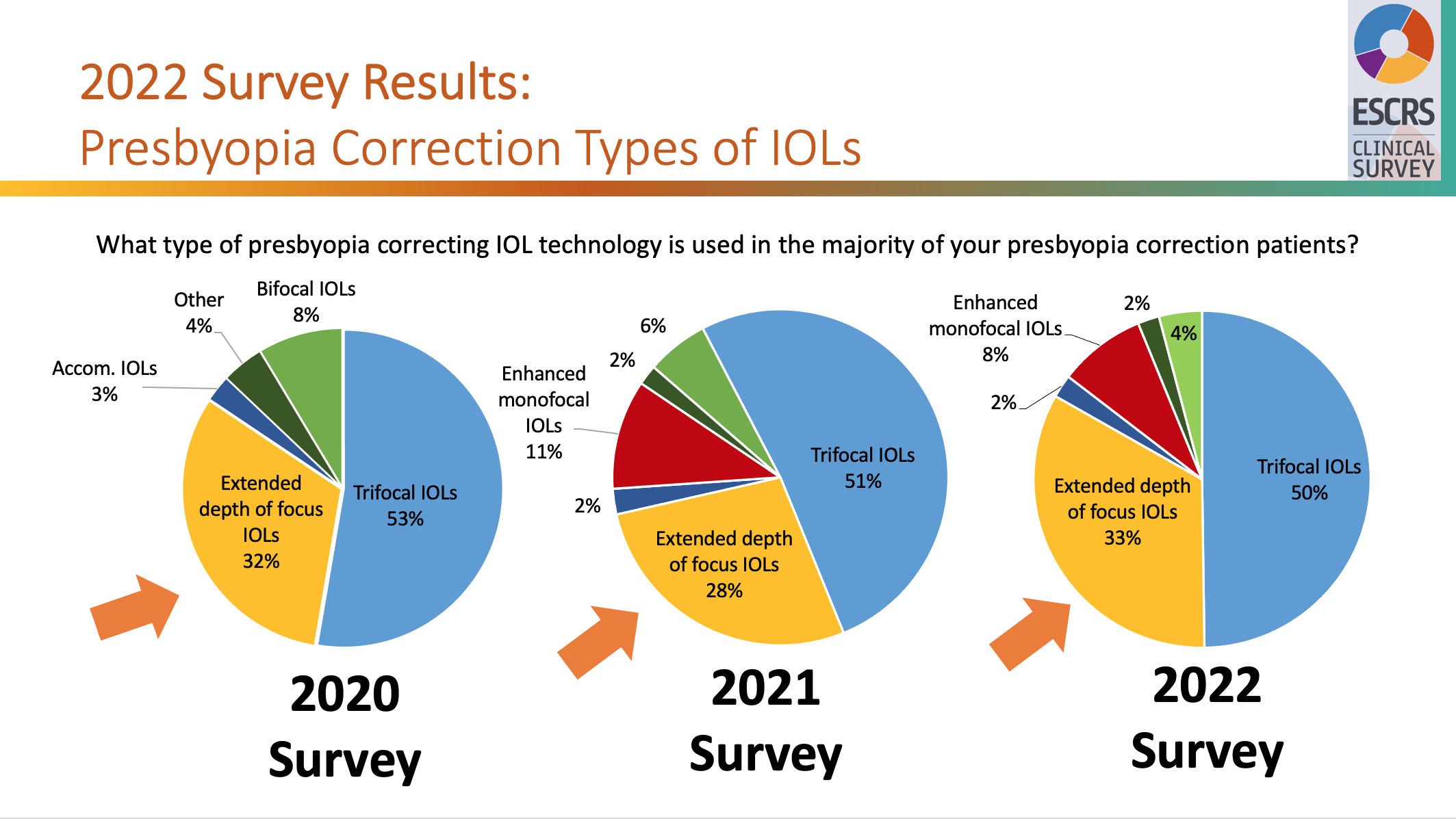
Eleven percent of respondents were implanting presbyopia-correcting IOLs, the same percentage as the previous year. Similarly, trifocal IOLs accounted for the same percentage as the previous year, 50% of cases. Extended depth of focus IOls saw a small increase to 33% from 28%. Accommodating and bifocal IOLs were used in 2% and 4% of cases, respectively.
Regarding their biggest concerns about performing more presbyopia-correcting IOL procedures, members cited cost to patient, concerns over contrast visual acuity, and night-time quality of vision. Twenty percent also expressed concerns about potential inadequate near-vision results.
Since 2016 there has been an 8% increase in cataract procedures using toric IOLs. The survey showed no clear consensus on the best approach in cases where the preoperative cylinder was 1.25 D or less. However, toric IOLS were the clear favourite in cases of astigmatism of at least 1.75 D.

The increased use of face masks in the wake of the COVID-19 pandemic is leading to a marked increase in dry eye symptoms and signs, according to a study presented here.
“Ophthalmologists should advise their patients of the potential ocular surface health risks related to face masks,” said Ana Pereira MD. “And fitting strategies should be adopted to try to minimize the discomfort associated with this condition.”
Dr Pereira’s study included 40 eyes of 20 health professionals with a mean age of 47 years old. An Ocular Surface Disease Index (OSDI) questionnaire assessed symptoms of dry eye disease. In each answer, the participants were asked to self-report the symptoms at two different times, pre- and post-COVID-19, when the use of face masks became generalised.
In addition, all volunteers underwent a non-invasive ocular surface workup using TearCheck® (ESW Vision) on the same day at two different times: at the beginning of the work shift before wearing a face mask, then again after six hours of continuous face mask use. The system calculated eye redness score (range 1–4), non-invasive break-up time (NIBUT), and tear meniscus thickness and tear film stability evaluation (TFSE) variation between the two measurements.
The results showed a mean increase in the OSDI score of 15.33 when comparing pre- and post-COVID-19 periods. Concerning the ocular surface parameters, eye redness score increased, tear meniscus thickness decreased, and NIBUT reduced after six hours of face mask use.
Advances in cataract surgery techniques and technologies combined with improved IOL designs and materials have lowered the rate of IOL exchange surgery and altered the percentages of its main indications, according to Matthias Gerl MD.
“IOL dislocation remains one of the most common indications for IOL explantation, followed by incorrect IOL power, patient dissatisfaction due to halos and glare, IOL opacification, and capsular contraction,” he said. “In the past, the principal indications for IOL exchange surgery were IOL dislocation, anterior uveitis, and unpredicted high refractive errors. However, IOL exchange surgery today appears to have a good safety profile and visual outcomes for the majority of these patients.”
Dr Gerl’s retrospective study included more than 26,000 eyes that underwent phacoemulsification with IOL implantation between 2016 and 2022. The cumulative incidence of IOL exchange was 2.2 per 1,000 cataract operations over six years. The main indication of IOL explantation was IOL dislocation in 24 cases (40.6%), followed by incorrect IOL power in 21 (35.6%), patient dissatisfaction due to halos and glare in 9 (15.3%), IOL opacification in 4 (6.8%) and capsular contraction in 1 (1.7%).
Glaucoma was the most common pre-existing ocular condition, accounting for 11 (18.6%) of all cases, followed by high myopia for 10 (16.9%), pseudoexfoliation syndrome for 6 (10.2%), diabetic retinopathy for 4 (6.8%), floppy iris for 5 (8.5%), and age-related macular degeneration for 3 (5.1%). The mean time interval between the cataract surgery and the IOL exchange was 10.5 months. The types of secondary implanted IOLs were monofocal IOLs in 32%, iris-claw in 30%, three-piece IOL in 20%, EDOF IOL in 13%, and multifocal IOLs in 3%. Vitreous prolapse was the most common intraoperative complication in 35%, and secondary cataract was the most common postoperative complication in 15% of cases.
Using telemedicine software seems to provide an effective, safe, and accurate means of following up with patients after routine cataract surgery, according to a study presented here.
“Our experience showed the video consultation was effective, safe, accurate, and satisfactory in this cohort of patients following routine cataract surgery,” said Lucia Pelosini MD. “There were no adverse effects or complications missed in the group subject to video consultation at two weeks compared to the patients reviewed in the clinic at the same period. The novel process of integrating remote video consultation to routine medical care resulted in favourable feedback from patients and offered the additional benefit of reduced hospital attendances and travelling expenses for patients.”
The telemedicine software (AOS, Advanced Ophthalmic Systems) allows the clinician to perform live video consultations, assess images of the anterior eye, and complete an interactive live visual acuity measurement following surgery.
Dr Pelosini’s study assessed the software in 65 patients two weeks after routine cataract surgery and compared this cohort with an equivalent group of patients who attended a face-to-face consultation after the same wait period.
The video consultation allowed a reliable symptom assessment, medication compliance, and external eye examination in all cases. The vast majority (97%) of patients said they were very satisfied with the video assessment, while 3% said they were satisfied with the consultation but experienced some technical difficulties in the connection. There was no adverse effect or missed postoperative complications in the group assessed by video consultation at final clinic review five weeks after surgery.
Ab-interno canaloplasty performed as a standalone procedure or combined with cataract surgery achieved a sustainable reduction in intraocular pressure (IOP) and medications in controlled and uncontrolled patients up to five years after surgery, according to Norbert Koerber MD.
“Uncontrolled patients’ IOP reduced significantly and was brought under control with no difference with controlled patients,” he said. “I must admit that I did not expect the results to be so good out to five years when I first started the study. However, we know from the ab-externo cases that it is a stable procedure over the long term.”
Dr Koerber’s retrospective single-centre case series study recruited 27 eyes of 22 patients with primary open-angle glaucoma (POAG) who had undergone canaloplasty using the iTrack microcatheter (Nova Eye Medical) via an ab-interno surgical technique (ABiC) with or without phacoemulsification. Patients were divided into two groups: IOP controlled with medications (less than 18mmHg) and uncontrolled (over 18mmHg). Primary efficacy endpoints included IOP and the number of glaucoma medications.
In the results, there was a 9% IOP reduction in the controlled group and a 42% reduction in the uncontrolled group at five years. More than 91% of patients had an IOP of less than 18mmHg at the five-year point. Medications also saw a sustained reduction over time, with a 29% reduction in the controlled group and a 36% reduction in the uncontrolled group at five years. Around one-third of patients (33%) were on zero medications at five years versus 4% at baseline.